Magic Mushrooms
‘They broke my mental shackles’: could magic mushrooms be the answer to depression?
From The Guardian
A liberty cap mushroom (Psilocybe semilanceata), known for its hallucinogenic properties, grows in a grassy fields where animal droppings occur in many moorlands throughout the UK the USA, Mexico and other countries.
New trials have shown the drug psilocybin to be highly effective in treating depression, with Oakland the latest US city to in effect decriminalise it last week. Some researchers say it could become ‘indefensible’ to ignore the evidence – but how would it work as a reliable treatment?
There are several more Magic Mushrooms – here are a couple more.
Lying on a bed in London’s Hammersmith hospital ingesting capsules of psilocybin, the active ingredient of magic mushrooms, Michael had little idea what would happen next. The 56-year-old part-time website developer from County Durham in northern England had battled depression for 30 years and had tried talking therapies and many types of antidepressant with no success. His mother’s death from cancer, followed by a friend’s suicide, had left him at one of his lowest points yet. Searching online to see if mushrooms sprouting in his yard were the hallucinogenic variety, he had come across a pioneering medical trial at Imperial College London. See Hallucinations Visions and Hallucinogens
Listening to music and surrounded by candles and flowers in the decorated clinical room, Michael anxiously waited for the drug to kick in. After 50 minutes, he saw bright lights leading into the distance and embarked on a five-hour journey into his own mind, where he would re-live a range of childhood memories and confront his grief. For the next three months, his depressive symptoms waned. He felt upbeat and accepting, enjoying pastimes he had come to feel apathetic about, such as walking through the Yorkshire countryside and taking photographs of nature.
“I became a different person,” says Michael. “I couldn’t wait to get dressed, get into the outside world, see people. I was supremely confident – more like I was when I was younger, before the depression started and got to its worst.”
The trial, finished in 2016, was the first modern study to target treatment-resistant depression with psilocybin, a psychedelic drug naturally occurring in around 200 species of mushroom. To varying degrees, Michael and all 18 other participants saw their symptoms reduce a week after two treatments, including a high, 25mg dose. Five weeks later, nine out of 19 patients found that their depression was still significantly reduced (by 50% or more) – results that largely held steady for three months. They had suffered from depression for an average of 18 years and all had tried other treatments. In January this year, the trial launched its second stage: an ambitious effort to test psilocybin on a larger group and with more scientific rigour (including a control group, which Michael’s study lacked), comparing the drug’s performance with escitalopram, a common antidepressant. The team has now treated about a third of the 60 patients and say that early results are promising for psilocybin.
Imperial’s current work is among a string of new studies that a group of professors, campaigners and investors hope will lead to psilocybin’s medical approval as a transformative treatment. Others soon to begin include an 80-person study run by Usona Institute, a Wisconsin-based medical non-profit, and a trial at King’s College London, as well as a 216-person trial that is already under way around the US, Europe and Canada, managed by the London-based life sciences company Compass Pathways. Robin Carhart-Harris, head of Imperial’s Centre for Psychedelic Research and a Compass scientific adviser, believes psilocybin could be a licensed medicine within five years, or potentially even sooner. “By about that point,” he says, “it would be like an irresistible force, and indefensible to ignore the weight of the evidence.”
Psilocybin mushrooms have been part of religious rituals for thousands of years. The Aztecs of Mexico referred to the mushroom as teonanácatl, or “God’s flesh”, in homage to its believed sacred power. In 1957, Albert Hoffman, a Swiss chemist working for the pharmaceutical company Sandoz, isolated psilocybin from the mushroom. Fifteen years earlier, he had accidentally ingested LSD, left work feeling dizzy, and experienced its psychedelic effects when he got home. During the 1960s, Sandoz sold psilocybin and LSD for research in medical trials, but the substances were soon outlawed after they became associated with the 60s counterculture.
Professor Robin Carhart-Harris at Imperial. Photograph: Graeme Robertson/The Guardian
Psilocybin remains in the most restricted category today under the UN Convention on Psychotropic Substances, the US 1970 Controlled Substances Act and the 1971 UK Misuse of Drugs Act, among others. David Nutt, a professor of neuropsychoparmacology at Imperial, who is overseeing the current trials, disputes the evidence for this, saying that heavily restricting the drug (and other psychedelics) has hindered research and propelled “lies” about its risks and medical potential. For him, the decision is “one of the most atrocious examples of the censorship of science and medicine in the history of the world”. (They have recently been accepted to use in the USA) See Psychedelics
If successful, the new wave of research may continue to change psilocybin’s reputation after decades of prohibition. Carhart-Harris believes the drug offers a better and more comprehensive treatment than current antidepressants, and that it could well be a powerful new therapy for a host of other mental illnesses, including anxiety and food disorders. A 2016 Johns Hopkins University study of 51 patients with life-threatening cancer showed high doses of psilocybin significantly reduced end-of-life depression and anxiety for six months in 80% of cases, and helped patients accept death; a New York University study that year showed similar results. Current trials are looking further at psilocybin’s potential for reducing smoking addiction and alcohol dependency, after initial pilots yielded powerful results. (Johns Hopkins researchers showed in a small study, for example, that 80% of heavy smokers had not smoked for a least a week, six months after psilocybin treatment.) See So What Happens When I Die?
Magic mushrooms ‘reboot’ the brain in depressed people.
Read more
Carhart-Harris thinks part of the reason the drug has been effective in treating depression in trials so far is that it can help people see their lives more clearly. When watching patients tripping, he often feels as if they see a truer version of reality than the sober therapists guiding them: “It is almost like being in the presence of someone particularly wise, in terms of what comes out of their mouth.” It is unclear how much of the depression alleviation comes from the psychiatric support surrounding the treatment. Either way, several patients have sourced top-ups independently since the first trial, as their depression has returned.
A room at Imperial College where patients take magic mushrooms. Photograph: Graeme Robertson/The Guardian
Much about the neuroscience of psychedelics remains unknown, but fMRI scans of patients’ brains after taking psilocybin showed reduced blood flow and resting activity in the amygdala, which is often overactive in depression and anxiety. They also show looser connections between brain networks, which then reintegrate in what the Imperial team suggests is part of the brain “resetting” itself on psilocybin. This may explain why the drug drives some patients to rethink entrenched beliefs and break compulsive thought patterns and behaviours. Imperial researchers believe that psilocybin operates differently from most current treatments. If common antidepressants dull emotions to help people cope, they theorise, psilocybin works on our serotonin system to heighten emotional responses and encourage people to actively confront their depression, which can prompt enduring shifts in mind-set.
For 48-year-old university design technician Kirk Rutter, this is why psilocybin seems to work – and why he hopes it will become medically available. He sees the drug not as a silver bullet but as a medicine that shows patients deep truths and requires them to apply teachings of this kind. Some other treatments, such as cognitive behavioural therapy, also seek to reshape thinking patterns, often in conjunction with antidepressants, but for many the current options fail to work. More than 300 million people suffer from depression globally, according to the World Health Organization, but researchers say that many of the most serious cases do not respond to antidepressants.
Magic mushrooms in capsule form. Photograph: Graeme Robertson/The Guardian
Rutter was in this group, having tried counselling and two prescription medicines in the five years before the Imperial trial, as his depression worsened following his mother’s death. After psilocybin, he began to break cycles of catastrophic thinking and had the confidence to make profound life changes, such as selling his house and moving away from abusive neighbours, reorganising his finances and travelling for enjoyment after years of not leaving the country. He says of psilocybin: “It removes any barriers and allows you to process what you need to in an almost seductive way. You are inevitably and irresistibly drawn into it.” One week after the treatment, he noticed a feeling of optimism come back to his life. “Hell,” he thought, “I haven’t had this for a long time.”
But it is hoped that the Compass trials will provide the evidence needed to get the drug medically approved for treatment-resistant depression. She founded the company with her husband, George Goldsmith, three years ago, after her son’s severe depression and OCD got progressively worse while he was being treated with traditional antidepressants in a top US hospital. He later recovered with the help of psilocybin therapy, and the company says it has now attracted around £28m in funding, including from the venture capitalist Peter Thiel, and has applied to patent a process to make psilocybin at scale. Some former Compass associates fear the company seeks to monopolise the psilocybin market and control medical access, criticisms that were aired last year by the US business website Quartz, although Malievskaia denies this.
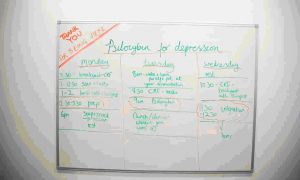
A noticeboard at Imperial College’s Centre for Psychedelic Research. Photograph: Graeme Robertson/The Guardian
Meanwhile, Compass hopes to request marketing authorisation for the drug within three years, if its trials are successful. It is proceeding slowly, though, having treated around six people since trials began in January, and Malievskaia says the process could take a decade until approval. She aims to accelerate progress, with new treatment sites recently opened at Columbia University, as well as in New Orleans and the Netherlands, among others.
Licensing is not the only obstacle to the drug becoming a common medicine. Taken over multiple hours in clinical settings with expert guides, psilocybin therapy does not come cheap. The new Imperial treatments cost more than £2,000 each, including doctors and therapists, and many patients could need multiple treatments each year for continued benefits. Malievskaia would not comment on how much Compass would plan to charge, but says she wants to maximise how many people can access the drug. Carhart-Harris says psilocybin therapy would be significantly more expensive than antidepressants and potentially more than counselling. “There is a cold reality to why selective serotonin reuptake inhibitors [antidepressants] dominate mental healthcare and that is that they are cheap,” he says.
The scientific, legal and commercial challenges may take years to be settled. But for many of the patients who have already been treated, and for some of the therapists guiding them, there is little doubt: it is only a matter of time before psilocybin and similar psychedelics reshape how we treat suffering – and understand our minds.
Magic mushrooms lift severe depression in clinical trial
Read more
Forty-year-old operations manager Melissa Elwin is among them. After an unpleasant first treatment, in which she felt trapped, during her second psychedelic trip inside Hammersmith Hospital, she felt as though she had left her body and was seeing her problems objectively. Psilocybin helped her confront her depression, fuelled by a difficult relationship and fraught breakup, and anxiety she had had since childhood. Under the drug, she started to find a resilience that has since helped her face her father’s death from dementia and a protracted legal battle with her ex-partner. Her descriptions of the trip are similar to the awe and unity Hoffman at times experienced on psychedelics while testing them: he saw in them a powerful ability to put our self and troubles in perspective.
“I was literally everywhere [during the psilocybin trip],” says Elwin. “In the most amazing nature scenes, like the orb of light twinkling through trees, in the ocean, in waterfalls. I had no recollection of time and I just wanted it to last for ever. For so long, I felt my depression was part of me, there was nothing I could do to change it. The antidepressants only made me feel drowsy and stopped me caring about things. This made me completely break my mental shackles. I returned to work [after being unemployed] and I was euphoric. I felt: I can do this, I can change my situation.”